Research Conducted by Chilean Physicians Has an Impact on Intensive Care Medicine Worldwide
Research on ANDROMEDA-Shock-2 was led by two Chilean academics from UC Chile, who coordinated with health professionals from 19 countries.
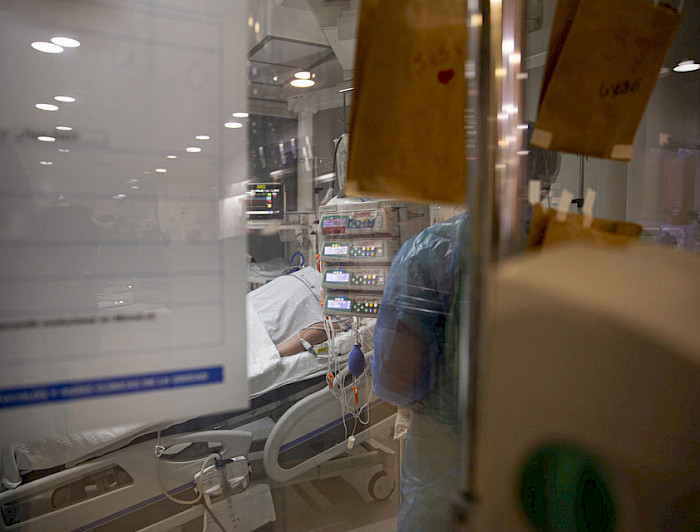
photo_camera Between six and eight hours is the window of time in which the intensivist, together with their team, work to minimize long-term complications in patients undergoing resuscitation. (Photo credits: Office of Media and Publications)
It was 2021, and the pandemic continued to complicate matters for patients in the intensive care unit. In the doctors’ lounge at the San Carlos de Apoquindo Clinic, Doctor Glenn Hernández, along with Doctor Eduardo Kattan, both intensivists and academics from the UC Chile Faculty of Medicine, reflected on how to create personalized strategies to guide the resuscitation of patients with sceptic shock as an alternative to the standard of care.
Patients with sceptic shock are those with the most serious infections. Organ failure due to lack of oxygenation and blood flow causes them to slowly begin to die. The medical team’s response is crucial. “Resuscitation means restoring circulation to normal levels, and this must be done within a few hours,” comments Dr Eduardo Kattan, as he explains his research.
Between six and eight hours is the window of time in which the intensivist, together with their team, work to minimize long-term complications in patients undergoing resuscitation, not only to save the patient’s life but also to ensure an optimal state for them to live. This is where ANDROMEDA-Shock-2 comes in, the concrete idea that began its journey in 2021 to guide a personalized resuscitation that improves quality of life, using simple signals at the patient’s bedside.

Global collaboration
An intuitive tool that does not require significant monitoring resources or laboratory tests. This is the goal that guided more than 800 collaborators from 19 countries in North America, South America, Europe and Asia.
By pressing on the index finger, as when playing with one’s fingertips, physicians Glenn Hernández and Eduardo Kattan saw how capillary refill time correlated with the normalization of blood flow and blood oxygenation. They gathered this type of study, tested on ANDROMEDA-Shock-1, to build the theoretical corpus of the project, which involved a total of 1,501 patients in 86 hospitals.
From Barros Luco Hospital to Quilpué Hospital in Chile, going all the way to Al-Amiri Hospital in Kuwait, intensivists faced logistical challenges: countries requesting insurance payments of over a thousand dollars per patient; platforms to ensure data protection, despite anonymity; questions about conducting studies at an intensive care unit (ICU), among others.
Despite the obstacles, the motivation to help hospitalized patients and their families was the driving force for the participating researchers. Thanks to their methodology, it was possible to reduce patients’ time spent on life support and resuscitated patients’ long-term complications. Volunteers, who received calls at 3:00 a.m. due to the time difference between the participating countries, met on Zoom to translate the protocols for use and used the fire emoji on Whatsapp to announce the inclusion of new patients in the study.
It was research that could be successful or unsuccessful. It involved the efforts of a team of different health professionals, took four years to complete, and raised many questions about whether to continue. This is where Dr Kattan justifies the team’s participation: “We achieved a collective effort, generating a renewed enthusiasm for the profession that sought not only to reach hospitals with advanced technologies, but also to provide an efficient, fast and effective resource for everyone, with a humanized approach.”
An essential commitment
Dr Hernández explains that the doctor-patient relationship is essential because that is where the heart of this project lies: individualizing therapy is key. By pressing the patient’s finger to evaluate physiological signals, including pulse, arterial and systolic pressure, treatment can be adjusted. Being able to restore the patient’s circulation and achieve efficient resuscitation ultimately translates into a shorter stay in the ICU; less time on mechanical ventilation; fewer days receiving dialysis and life support. “And, most importantly, fewer hours of distress for families,” adds Hernández.
There are no additional costs other than human dedication. “This protocol does not involve any additional expense for the patient or for the hospital. There are none,” notes the intensivist, which means that this is an accessible tool and a change in public health. Reducing time on life support for patients undergoing resuscitation due to sceptic shock means having more ICU beds available for other patients who need them.
On October 29, the ANDROMEDA-Shock-2 team achieved the publication of their research in the Journal of the American Association (JAMA), one of the three most important scientific journals in the field of medicine. This marks a key milestone for intensive care medicine and for UC Chile, where research with the potential to transform health is being conducted from the southernmost part of the American continent. “This study will have a global impact and will undoubtedly change the way patients in sceptic shock are resuscitated in intensive care,” concludes Dr Kattan.


